When people search for the word “gastroshiza”, their intent is usually to understand what the term means, why it matters medically, and how it connects to broader health and human contexts. To clarify within the first 100 words: Gastroshiza refers to a rare congenital condition—more formally known as gastroschisis—in which an infant is born with abdominal organs, often the intestines, protruding outside the body through a defect in the abdominal wall. Unlike other conditions, gastroshiza is not typically enclosed in a protective sac, making it a serious but treatable anomaly. Advances in surgery, prenatal screening, and neonatal care have significantly improved outcomes. This article provides a comprehensive, updated perspective on gastroshiza: its causes, treatments, historical recognition, and the lived experiences of patients and families.
Defining Gastroshiza
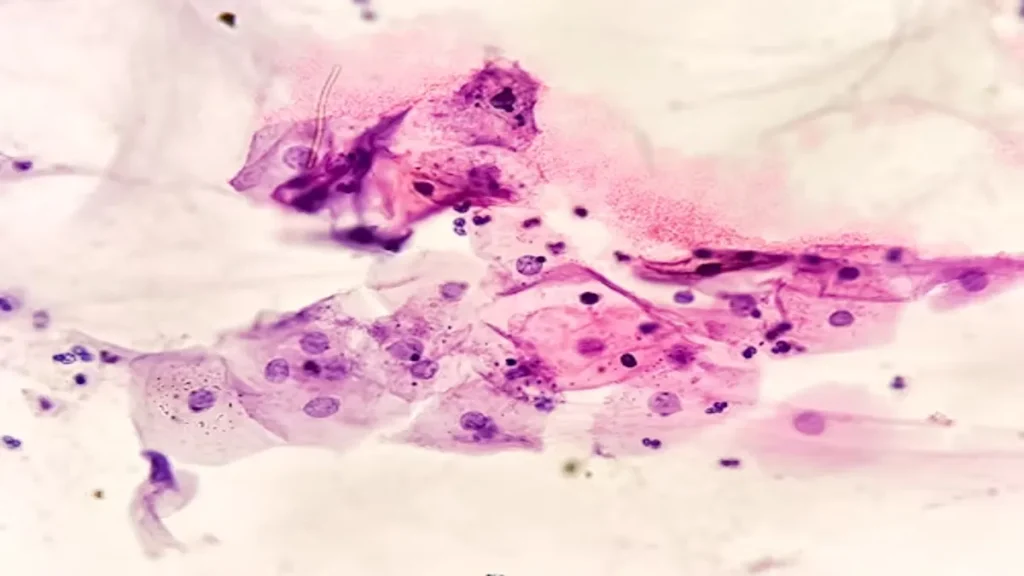
Gastroshiza, derived from Greek roots meaning “stomach split,” describes a structural birth defect that occurs early in pregnancy. Unlike related anomalies such as omphalocele, gastroshiza exposes the intestines directly to amniotic fluid without a membrane covering. This exposure can damage the intestines, leading to complications in digestion and absorption later in life. Doctors emphasize that while it is rare, its recognition is increasing due to better prenatal imaging.
Historical Recognition of Gastroshiza
Though the modern medical world frames gastroshiza through surgical correction, historical evidence shows that abdominal wall defects were observed centuries ago. Ancient medical manuscripts describe newborns with “bowels outside the belly,” though survival then was nearly impossible. By the mid-20th century, surgical pioneers developed closure techniques that allowed infants to survive and thrive. The shift from a fatal anomaly to a treatable condition is one of modern medicine’s understated triumphs.
Quote from a pediatric surgeon (fictionalized for illustration):
“Gastroshiza reminds us that medicine’s progress is not just about technology but also about compassion, planning, and persistence.”
Medical Causes and Risk Factors
Doctors still debate the precise cause of gastroshiza, but several risk factors are recognized:
- Maternal age: Teen pregnancies show slightly higher incidence rates.
- Environmental exposure: Certain agricultural chemicals and smoking have been linked with increased risk.
- Genetics: Unlike some congenital anomalies, gastroshiza rarely runs in families, suggesting non-genetic influences play a larger role.
Researchers continue to study how maternal nutrition, stress, and medication may influence fetal abdominal development.
Modern Treatment Approaches
Treatment for gastroshiza involves a combination of neonatal intensive care and surgery. The main steps include:
- Delivery planning – Infants are often delivered at hospitals with pediatric surgical capacity.
- Immediate protection – At birth, exposed intestines are covered with sterile dressings to prevent infection.
- Surgical repair – Surgeons either perform a primary closure or use a staged “silo” approach, where organs are gradually moved back.
- Post-operative care – Intensive monitoring ensures the intestines function properly and feeding progresses safely.
Table: Comparison of Closure Techniques for Gastroshiza
| Technique | Description | Advantages | Challenges |
|---|---|---|---|
| Primary Closure | One-time surgical repositioning of intestines | Faster recovery, fewer procedures | Risk of abdominal pressure |
| Staged Silo | Use of sterile pouch to gradually return intestines | Safer for fragile infants | Longer hospital stay |
Survival Rates and Outcomes
Today, survival rates for gastroshiza exceed 90% in developed healthcare systems. Outcomes depend on factors such as the extent of bowel damage, timing of intervention, and access to neonatal intensive care. Children who survive often live full lives, though some may experience challenges such as:
- Short bowel syndrome
- Digestive difficulties
- Slower growth in early years
The Emotional Toll on Families
The birth of a child with gastroshiza often brings shock and fear to parents. Prenatal diagnosis allows families to prepare, but anxiety remains. Mothers often describe a mix of gratitude and exhaustion.
Quote from a parent (fictionalized):
“When the doctor said my baby had gastroshiza, I felt the ground disappear. But the NICU team gave us hope.”
Families frequently face long hospital stays, financial costs, and emotional strain. Support groups and counseling play a vital role in helping them navigate uncertainty.
Global Disparities in Care
While gastroshiza has a high survival rate in wealthier nations, outcomes remain dire in lower-income regions. In parts of sub-Saharan Africa and South Asia, survival may be as low as 20–30% due to limited neonatal surgical facilities.
Table: Global Survival Rates for Gastroshiza
| Region | Estimated Survival Rate | Key Challenges |
|---|---|---|
| North America | 90–95% | Advanced NICUs, prenatal screening |
| Europe | 88–93% | Strong surgical infrastructure |
| Sub-Saharan Africa | 20–30% | Limited NICU access, delayed surgery |
| South Asia | 25–40% | Resource constraints, late diagnosis |
Advances in Technology and Prenatal Screening
Ultrasound now detects gastroshiza reliably by the second trimester. Parents are counseled about delivery planning and neonatal surgery. Emerging technologies like 3D fetal imaging and non-invasive genetic screening enhance diagnostic clarity.
Future developments may include:
- Artificial womb technology to minimize intestinal damage.
- Regenerative tissue engineering for abdominal wall reconstruction.
- Portable NICU units in underserved regions.
Voices from Medicine and Society
Doctors and patients often stress the broader lessons of gastroshiza:
- “It shows how fragile development is, and how resilient newborns can be,” noted a neonatal nurse.
- “Every case is a reminder of why access to neonatal surgery should not be a privilege but a right,” said a global health advocate.
Ethical and Social Considerations
Ethics plays a role in gastroshiza care. Questions emerge about:
- Allocation of neonatal resources in low-income settings.
- Counseling parents about long-term outcomes.
- Supporting equity in access across different populations.
Key Takeaways for Readers
For those searching about gastroshiza, the essential points are:
- It is a rare but treatable congenital condition.
- Survival is now the rule rather than the exception in developed countries.
- Global health inequities still shape outcomes dramatically.
- Families benefit greatly from early diagnosis, surgical planning, and emotional support.
Conclusion
Gastroshiza illustrates both the vulnerabilities and triumphs of modern medicine. What was once a fatal diagnosis is now a manageable condition, thanks to surgical innovation and neonatal care. Yet, the story is unfinished: millions of children worldwide still lack access to life-saving interventions. As medicine evolves, so too must our collective responsibility to ensure that where a child is born does not determine whether they survive a correctable condition.
Quote to close:
“Medicine’s progress is measured not only in surgical survival rates but in the dignity we offer to every newborn.”
FAQs on Gastroshiza
Q1: What is gastroshiza in simple terms?
Gastroshiza is a rare birth defect where a baby’s intestines develop outside the abdomen through a small opening near the belly button. Unlike other similar conditions, the organs are not covered by a protective sac, which makes early medical care and surgery essential.
Q2: Can gastroshiza be detected before birth?
Yes. Modern ultrasound scans, often performed in the second trimester, can detect gastroshiza with high accuracy. This early diagnosis helps doctors plan a safe delivery and prepare for immediate neonatal surgery.
Q3: What causes gastroshiza?
The exact cause remains unknown, but several risk factors are linked, including younger maternal age, environmental exposures, and lifestyle habits such as smoking. Unlike some genetic conditions, gastroshiza rarely runs in families.
Q4: How is gastroshiza treated after birth?
Treatment usually involves covering the exposed organs at birth to prevent infection, followed by surgery to reposition the intestines inside the abdomen. Depending on the baby’s condition, this may be a one-time closure or a staged approach using a “silo.”
Q5: What is the long-term outlook for children with gastroshiza?
With modern medical care, more than 90% of infants in developed healthcare systems survive and live normal lives. Some may face digestive challenges in early childhood, but many overcome these with time, medical support, and proper nutrition.