Millions of Americans live with leg pain, cramping, and cold extremities without realizing these symptoms could signal a serious vascular condition. Peripheral arterial disease (PAD) affects 1 in every 20 Americans over age 50, yet many cases go undiagnosed or are mistakenly attributed to arthritis or nerve problems.
Understanding your peripheral arterial disease treatment options can make the difference between maintaining an active lifestyle and facing serious complications. Modern medical advances have revolutionized how we approach PAD, offering minimally invasive solutions that restore blood flow and relieve symptoms with minimal downtime.
This comprehensive guide explores everything you need to know about PAD treatment, from recognizing early symptoms to understanding the latest therapeutic approaches that can help you regain mobility and improve your quality of life.
Understanding Peripheral Arterial Disease
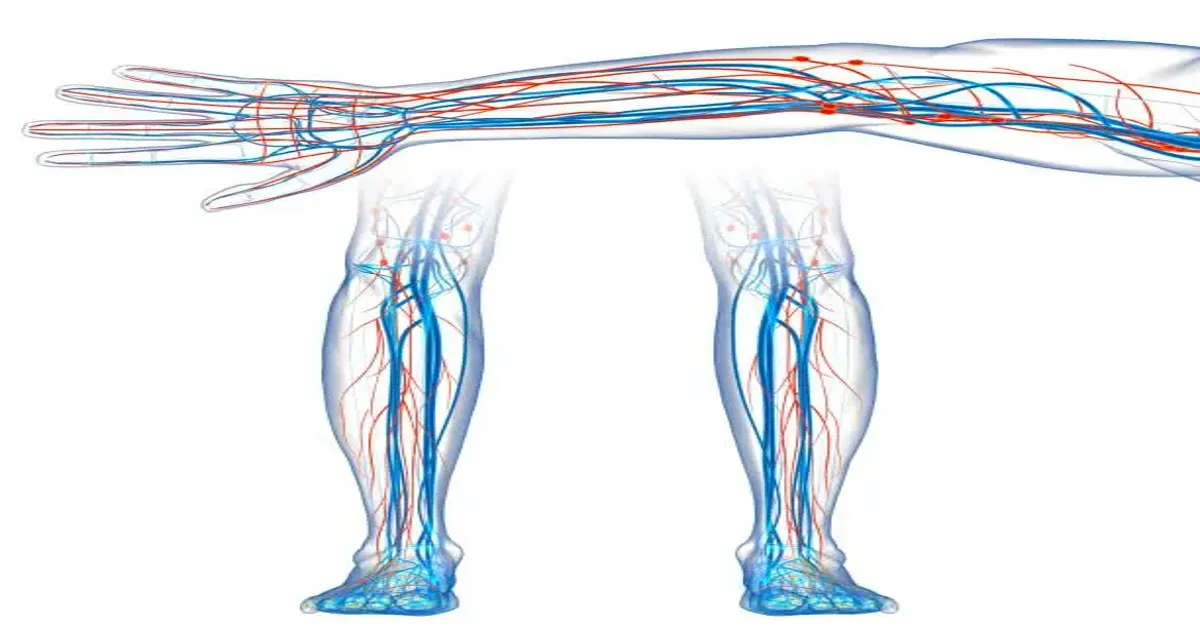
Peripheral arterial disease occurs when plaque composed of cholesterol and calcium accumulates in the arteries that supply blood to your extremities. This buildup narrows the arteries and reduces blood flow through a process called atherosclerosis, commonly known as “hardening of the arteries.”
The condition primarily affects the legs and feet, though it can impact other areas of the body. When your muscles don’t receive adequate blood flow, they struggle to function properly, leading to pain, cramping, and other uncomfortable symptoms.
PAD represents more than just a circulation problem. Patients with this condition face an increased risk of heart attack and stroke, making early detection and treatment essential for overall cardiovascular health.
Recognizing PAD Symptoms
Early recognition of PAD symptoms enables prompt treatment and better outcomes. The condition often develops gradually, and symptoms may be subtle at first.
Common Early Signs
The most frequent early symptom involves pain, numbness, or heaviness in your legs, particularly when walking or climbing stairs. This discomfort, known as intermittent claudication, occurs because your muscles aren’t receiving enough oxygen-rich blood during physical activity.
Many patients describe this sensation as cramping or aching that improves with rest. The pain typically affects the calves but can also occur in the thighs, hips, or buttocks, depending on which arteries are affected.
Advanced Symptoms
As PAD progresses, symptoms become more severe and may include:
- Burning pain in the toes and feet during rest or sleep
- Non-healing sores or wounds on legs, feet, and toes
- Color changes in feet, with skin appearing pale or blue
- Reduced nail growth and decreased hair growth on legs and toes
- In men, erectile dysfunction, especially when combined with diabetes
These advanced symptoms require immediate medical attention, as they indicate severely compromised blood flow that could lead to serious complications.
Risk Factors and Causes
Several factors increase your likelihood of developing PAD. Understanding these risk factors helps you take preventive measures and seek appropriate medical care.
Controllable Risk Factors
Smoking represents the most significant modifiable risk factor for PAD. Tobacco use damages blood vessel walls and accelerates plaque formation. Quitting smoking dramatically reduces your risk and slows disease progression.
Diabetes significantly increases PAD risk by damaging blood vessels and accelerating atherosclerosis. Maintaining good blood sugar control through diet, exercise, and medication helps prevent or slow PAD development.
High blood pressure and elevated cholesterol levels contribute to plaque formation in arteries. Managing these conditions through lifestyle changes and medication reduces your PAD risk.
Non-Controllable Risk Factors
Age plays a significant role in PAD development, with risk increasing substantially after age 50. Men typically develop PAD earlier than women, though post-menopausal women face similar risks.
Family history of cardiovascular disease, including PAD, heart disease, or stroke, increases your likelihood of developing the condition. Certain ethnic groups, including African Americans, also face higher PAD risks.
Diagnostic Approaches
Accurate diagnosis forms the foundation of effective peripheral arterial disease treatment. Vascular specialists use several advanced diagnostic tools to assess blood flow and identify arterial blockages.
Ankle-Brachial Index (ABI)
The ABI test compares blood pressure measurements in your ankles and arms. This simple, non-invasive test provides valuable information about blood flow to your legs and can detect PAD even before symptoms appear.
Imaging Studies
Doppler ultrasound creates detailed images of blood flow through your arteries, helping identify blockages and assess their severity. This painless test provides real-time information about circulation in your legs.
More advanced imaging techniques, such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA), create detailed pictures of your blood vessels, allowing physicians to plan targeted treatments.
Specialized Testing
Treadmill testing may be performed to assess how your symptoms respond to exercise and measure the distance you can walk before experiencing pain. This information helps determine disease severity and treatment effectiveness.
Conservative Treatment Options
Many patients benefit from conservative peripheral arterial disease treatment in Houston approaches, especially when the condition is caught early. These non-invasive strategies focus on improving circulation and managing symptoms through lifestyle modifications and medications.
Lifestyle Modifications
Regular exercise represents one of the most effective treatments for PAD. A structured walking program can improve circulation, reduce symptoms, and enhance overall cardiovascular health. Most patients should aim for 30-45 minutes of walking, three to five times per week.
Smoking cessation is crucial for all PAD patients. Tobacco use significantly worsens circulation and accelerates disease progression. Various smoking cessation programs and medications can help you quit successfully.
Dietary changes that reduce cholesterol and control blood sugar levels support improved vascular health. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients while limiting harmful fats and excessive sodium.
Medication Management
Several medications can improve PAD symptoms and slow disease progression. Antiplatelet drugs, such as aspirin or clopidogrel, reduce blood clot formation and improve circulation.
Cholesterol-lowering medications, particularly statins, help prevent further plaque buildup and may even reduce existing deposits. These drugs provide cardiovascular benefits beyond PAD treatment.
Cilostazol, a medication specifically approved for PAD, can improve walking distance and reduce leg pain in some patients. This drug works by improving blood flow and reducing inflammation.
Minimally Invasive Treatment Procedures
When conservative treatments aren’t sufficient, modern minimally invasive procedures offer effective solutions with reduced recovery times compared to traditional surgery.
Angioplasty
Angioplasty involves inserting a small balloon into the blocked artery and inflating it to compress plaque against the vessel wall, restoring blood flow. This procedure is performed under local anesthesia and typically requires only a small incision.
The balloon is guided to the blockage using advanced imaging technology, allowing for precise treatment of affected areas. Most patients can return home the same day and resume normal activities within a few days.
Stenting
Stenting often accompanies angioplasty to maintain arterial openness. A small wire mesh tube called a stent is placed in the treated artery to prevent it from narrowing again.
Modern stents are designed to integrate with your natural artery wall over time, providing long-term support for improved blood flow. Some stents are coated with medications that help prevent re-blockage.
Atherectomy
Atherectomy involves removing plaque from artery walls using specialized cutting devices. This technique is particularly useful for heavily calcified blockages that might not respond well to angioplasty alone.
The procedure precisely removes plaque while preserving healthy artery wall tissue. Different atherectomy devices are available to address various types of blockages and artery locations.
Endovascular Therapy
Endovascular therapy encompasses various catheter-based treatments that restore circulation from inside the blood vessel. These procedures use advanced imaging guidance to deliver targeted treatment to specific areas of blockage.
This approach offers several advantages, including reduced procedural risks, shorter recovery times, and the ability to treat multiple blockages during a single session.
Wound Care and Healing Support
Patients with advanced PAD often develop non-healing wounds or ulcers on their feet and legs. Effective peripheral arterial disease treatment must address both the underlying circulation problem and wound healing support.
Improving Blood Flow for Healing
Restoring adequate blood flow to affected areas is essential for wound healing. The minimally invasive procedures described above can dramatically improve healing rates by delivering oxygen and nutrients to damaged tissue.
Comprehensive Wound Management
Specialized wound care protocols help prevent infection and promote healing. This may include regular wound cleaning, appropriate dressing selection, and infection control measures.
Advanced wound care techniques, such as negative pressure therapy or bioactive dressings, can accelerate healing in difficult cases. These approaches work best when combined with improved circulation through vascular intervention.
Preventing PAD Complications
Untreated PAD can lead to serious complications, including non-healing ulcers, infections, and even amputation. Early intervention and ongoing management significantly reduce these risks.
Regular Monitoring
Patients with PAD require regular follow-up care to monitor disease progression and treatment effectiveness. This includes periodic ABI testing, symptom assessment, and medication adjustments.
Infection Prevention
Proper foot care becomes crucial for PAD patients, as poor circulation increases infection risk. Daily foot inspection, appropriate footwear, and prompt treatment of minor injuries help prevent serious complications.
Cardiovascular Risk Management
Since PAD increases heart attack and stroke risk, comprehensive cardiovascular care is essential. This includes blood pressure control, cholesterol management, and diabetes care when applicable.
Choosing the Right Treatment Approach
The best peripheral arterial disease treatment depends on several factors, including symptom severity, blockage location, overall health status, and personal preferences. A comprehensive evaluation by a vascular specialist helps determine the most appropriate approach.
Factors in Treatment Selection
Disease severity plays a major role in treatment selection. Patients with mild symptoms may benefit from conservative management, while those with severe blockages or non-healing wounds typically require intervention.
Blockage location and characteristics influence procedure selection. Some areas respond better to specific techniques, and severely calcified blockages may require specialized approaches.
Personalized Treatment Plans
Effective PAD treatment requires individualized care that considers your unique circumstances, goals, and preferences. A skilled vascular specialist will work with you to develop a treatment plan that addresses your specific needs and lifestyle requirements.
Recovery and Long-term Management
Successful peripheral arterial disease treatment extends beyond the initial intervention. Long-term management strategies help maintain improvements and prevent disease progression.
Post-Procedure Care
Most minimally invasive procedures require minimal recovery time, with many patients returning to normal activities within days. Following post-procedure instructions carefully helps ensure optimal healing and results.
Ongoing Lifestyle Management
Continuing healthy lifestyle habits remains crucial for long-term success. Regular exercise, smoking cessation, and proper nutrition support continued vascular health and may prevent future blockages.
Regular Follow-up Care
Scheduled follow-up appointments allow your healthcare team to monitor your progress, adjust medications as needed, and detect any new problems early. This ongoing relationship is essential for maintaining optimal vascular health.
Finding Relief Through Expert Care
Peripheral arterial disease treatment has advanced significantly, offering hope for patients who previously faced limited options. Modern minimally invasive procedures provide effective solutions with reduced risks and faster recovery times compared to traditional surgery.
Early diagnosis and treatment are key to preventing serious complications and maintaining an active lifestyle. If you’re experiencing leg pain, cramping, or other symptoms that might indicate PAD, don’t wait to seek evaluation from a vascular specialist.
The combination of advanced diagnostic tools, proven treatment techniques, and comprehensive care approaches means that most PAD patients can achieve significant symptom improvement and better quality of life. With proper treatment and ongoing management, you can take control of your vascular health and return to the activities you enjoy.